Hope for schizophrenia patients after discovery of brain cells associated with this mental chronic disorder
There are limited studies underlying the basis of schizophrenia that can be used to model experiments to expand the genomic basis of schizophrenia and help alleviate its symptoms more effectively then the treatments available today. That is exactly what a recent study has discovered. This study incorporated knowledge of the brain from single-cell RNA sequencing and analyzed whether specific loci associated with schizophrenia were mapped on specific cells in the brain.
Author: Petru Buracioc
Download: [ PDF ]
Neuroanatomy
Schizophrenia is one of diverse mental disorders affecting millions of people with minimal scientific and genetic basis which impedes experimental modeling that can successfully alleviate its symptoms with minimal side effects. Finding the genetic basis of this neurological disorder is important in understanding more about schizophrenia and other similar neurological disorders. In a paper recently published in Nature Genetics, Nathan Skene and other neuroscientists investigate the brain cell types that are involved in schizophrenia. The primary finding of this article is the specific cell types in the brain associated with schizophrenia and how each cell correlates with this psychiatric disease using information about the brain from singlecell RNA sequencing.
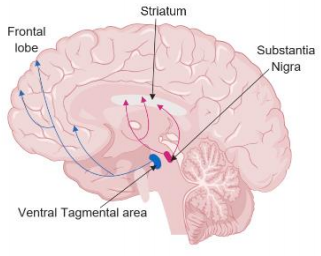
Schizophrenia is a psychotic illness described by delusions, hallucinations, and bizarre behavior. schizophrenia symptoms could be negative and positive. Negative symptoms involve the reduced expression of emotions, memory impairment, difficulty, and difficulty initiating goal-directed behavior. Positive symptoms include delusion, hallucinations, and disorganized behavior.1 One of the neuromodulatory systems in the brain that is responsible for symptoms in schizophrenia is dopamine. Dopaminergic pathway especially the one described in figure 1 is found to be abnormal as well as the prefrontal cortex where the principal cells are pyramidal cells among schizophrenic patients.2
The data used in this study was the human-mouse homolog list. The cell-type specificity or the genes correlating to certain cells was calculated using a metric system. MAGNA, a program used for gene set analysis was used to analyze the association for gene-level schizophrenia statistics to the cell-type-specific expression. Whether the brain cell types were associated with schizophrenia, CLOZUK which is a genome-wide association finding was used. Cell-type specificity of gene expression was determined from the scRNA-seq data from Karolinska Institutet. The brain regions identified from the genome associations with schizophrenia in this study were determined to be neocortex, striatum, hippocampus, hypothalamus, and midbrain.3
This study found clear connections between human genomic findings for schizophrenia in multiple studies and specific brain cell types using single-cell RNA sequencing. Four cells out of 24 main brain cell types were found to have clear connections to schizophrenia. These cells are MSNs, pyramidal cells in hippocampal CA1, pyramidal cells in the somatosensory cortex and cortical interneurons which were determined to play significant roles in schizophrenia.3
This study is significant because it connects the genome findings for schizophrenia and specific cell types, opening the door for a deeper understanding of the cells associated with this disease. With the results of this study, in vivo and in vitro experiments could be done to study the genes that produce the symptoms of Schizophrenia. Since Schizophrenia is associated with memory dysfunction and decreased cognitive function, therefore, parts of the brain such as the neocortex, hippocampus, and the hypothalamus are involved in schizophrenia as concluded with the cells identified in this study. Additionally, taking into consideration the dopamine hypothesis associated with schizophrenia that increased dopamine pathways increase symptoms of this disorder could lead to a better understanding of the basis of schizophrenia and how what can be done to help alleviate the symptoms of schizophrenia.
[+] References
Bear, M. F., Connors, B. W., Paradiso, M. A. (2016). Neuroscience: Exploring the Brain, Fourth Edition Waddington, J. L. (1993). Schizophrenia: developmental neuroscience and pathobiology. The Lancet, 341(8844), 531-532.
Meyer-Lindenberg A., Reduced prefrontal activity predicts exaggerated striatal dopaminergic function in schizophrenia. Nature Neuroscience volume 5, pages267–271. https://doi.org/10.1038/nn804
Skene N.G., Genetic identification of brain cell types underlying schizophrenia. Nature Genetics volume 50, pages825–833 (2018), https://doi.org/10.1038/s41588-018-0129-5
Ranganath, C., Minzenberg, M. J., & Ragland, J. D. (2008). The cognitive neuroscience of memory function and dysfunction in schizophrenia. Biological psychiatry, 64(1), 18-25
Paz, R. D., Tardito, S., Atzori, M., & Tseng, K. Y. (2008). Glutamatergic dysfunction in schizophrenia: from basic neuroscience to clinical psychopharmacology. European neuropsychopharmacology, 18(11), 773-786
Seeman, P. (1987). Dopamine receptors and the dopamine hypothesis of schizophrenia. Synapse, 1(2), 133-152
Jentsch, J. D., & Roth, R. H. (1999). The neuropsychopharmacology of phencyclidine: from NMDA receptor hypofunction to the dopamine hypothesis of schizophrenia. Neuropsychopharmacology, 20(3), 201-225
[+] Other Work By Petru Buracioc
A new drug approach increases cognition in rats
Neurophysiology
In a new study the α4β2 nicotinic acetylcholine receptors, a subtype of nicotinic acetylcholine receptors was studied in relation to their role in attention and cognition. This research presents a novel approach using a positive allosteric modulator on α4β2 nicotinic acetylcholine receptors to increase cognition in rats. This approach can be used in cognitive deficit disorders such as Alzheimer’s Disease and schizophrenia, which show a reduction of α4β2 nicotinic acetylcholine receptors in several parts of the brain.
The interactive role of Aβ plaques and tau pathology and their effects in Alzheimer’s disease
Neuroscience In Review