A study of neuronal distribution within the brain of epileptic patients shows the preservation of a certain neuron
A new study finds a link between distribution patterns of neurons within the brain and tissue samples from epileptic patients, indicating that a certain interneuron is mainly preserved in the epileptic brain.
Author: Ashlynn Dean
Download: [ PDF ]
Neurophysiology
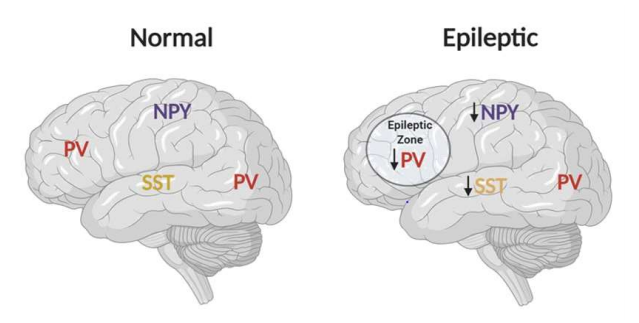
Although epileptic brains are commonly studied, the specific distribution patterns of biological markers within these brains have not been highly studied. In a paper recently published by Neuroscience, Zhu et al. (2018) investigate the distribution of neurons and certain biological markers within the brain of epileptic patients.1 This study found that somatostatin (SST) and neuropeptide Y-containing (NPY) neurons were reduced in the epileptic brain while Parvalbumin-positive (PV) interneurons were mainly conserved within the brain of epileptic patients, indicating that these neurons do not experience damage in the majority of the brain.
Introduction
Epilepsy is a broad spectrum of brain disorders that can range from benign to life-threatening and disabling.2 There are multiple mechanisms to seizures, but all mechanisms revolve around the idea that there is an imbalance in neuronal activity within the brain.3 The effect of seizures on neurons, especially severe or repeated seizures, has been highly researched and debated for many years.4 It is widely accepted that neuronal death can result from prolonged seizures.5 There is also evidence that brief seizures can cause some form of neuronal death, but this knowledge is not as well accepted.5 Some studies have focused on a specific set of neurons, called interneurons, and found that this group was highly involved in seizures and were especially susceptible to damage from epileptic seizures.6,7 Interneurons are a subset of neurons that have the purpose of inhibiting or exciting other neurons. Much research is devoted to finding markers within the brain that relate to the cause and severity of epilepsy, but not many have researched the distribution and conservation of certain neurons within the epileptic brain. In this study, the neurons focused on are Parvalbumin (PV), somatostatin (SST), cholecystokinin (CCK), tyrosine hydroxylase (TH), and neuropeptide Y-containing interneurons (NPY).
Methods
Brain tissue was removed from 9 patients while undergoing surgery to treat an epileptic condition and 3 patients undergoing non-epilepsy related brain surgery. This tissue was then frozen and sectioned into thin slices. These slices were stained with substances that made each type of interneuron a different color, indicating different cell components including PV, SST, CCK, TH, and NPY. Each type of interneuron was counted within each brain layer and the distribution of each of these interneurons was noted as well. The number of neurons with more than one labeled cellular component was also recorded (double-labeled cells).
Results
It was found that SST, PV, and CCK cells were found in the middle and deep layers of the brain, while TH and NPY cells were generally found deeper. Groups of neurons contained similar double-labeling patterns including PV + TH, PV + CCK, SST + NPY, and SST + TH. Both SST and NPY cells showed reduced densities than in the average non-epileptic brain (Figure 1). As for PV cells, it was found the overall density and number of PV cells remained the same between epileptic and non-epileptic brain tissue. In the main epileptic zones of the epilepsy brains, it was found that there were a lower PV density and number than the rest of the brain and compared to non-epileptic brain tissue (Figure 1).
Discussion
These data indicate that multiple types of interneurons are affected by epileptic conditions within the brain. Both SST and NPY cell densities are lowered in the epileptic brain compared to the non-epileptic brain. These two types of cells have been shown to previously be important in the generation of brain network activity and seizure-like activity.8 The reduction of SST and NPY cells may indicate damage to these cells in the brains of epileptic patients. PV cells were reduced in the epileptic zones but maintained in the rest of the brain within patients with epilepsy. PV-containing neurons have the function of inhibiting, or slowing the activity, of other neurons.9,10,11 The lowered intensity of inhibiting neurons in epileptic patients corresponds with the high activity of neurons during seizures. Other studies have found that the intensity of PV cells was also reduced in certain sections, including both frontal and middle, of the epileptic brain.12 Because of the relationship between PV cells and epilepsy, these data indicate that PV cells are a good target for epilepsy treatment. Targeting PV cells should provide more information on the mechanism of damage to PV cells due to seizures. Future studies should focus on ways to restore PV-containing neurons as a possible treatment for recurrent seizures and epilepsy or create formulas to prevent PV loss during future seizures.
[+] References
Zhu, Q., Ke, W., He, Q., Wang, X., Zheng, R., Li, T., Luan, G., Long, Y., Liao, W., Shu, Y. (2018). Laminar Distribution of Neurochemically-Identified Interneurons and Cellular Co-expression of Molecular Markers in Epileptic Human Cortex. Neuroscience, 34(6), 992-1006.
National Institute of Neurological Disorders and Stroke: NINDS (2019). Epilepsy Information Page. https://www.ninds.nih.gov/Disorders/All-Disorders/Epilepsy-Information-Page.
Scharfman, H. E. (2007). The Neurobiology of Epilepsy. Current Neurology and Neuroscience Reports, 7(4), 348-354.
Dingledine, R., Varvel, N. H., Dudek, F. E. (2014). When and How Do Seizures Kill Neurons, and Is Cell Death Relevant to Epileptogenesis? Advances in Experimental Medicine and Biology, 813, 109-122.
Berdichevsky, Y., Dzhala, V., Mail, M., Staley, K. J. (2012). Interictal spikes, seizures and ictal cell death are not necessary for post-traumatic epileptogenesis in vitro. Neurobiology of Disease, 45(2), 774-785.
Marx, M., Haas, C. A., Haussler, U. (2013). Differential vulnerability of interneurons in the epileptic hippocampus. Frontiers in Cellular Neuroscience, 7, 167.
Jiang, X., Lanchance, M., Rossignol, E. (2017). Involvement of cortical fast-spiking parvalbumin-positive basket cells in epilepsy. Progress in Brain Research, 226, 81-126.
Yekhlef, L., Breschi, G. L., Lagostena, L., Russo, G., Taverna, S. (2015). Selective activation of parvalbumin or somatostatin-expressing interneurons triggers epileptic seizurelike activity in mouse medial entorhinal cortex. Journal of Neurophysiology, 113, 1616-1630.
Silberberg, G. & Markram, H. (2007). Disynaptic inhibition between neocortical pyramidal cells mediated by Martinotti cells. Neuron, 53, 735-746.
Ren, M., Yoshimura, Y., Takada, N., Horibe, S., Komatsu, Y. (2007). Specialized inhibitory synaptic actions between nearby neocortical pyramidal neurons. Science, 316, 758-761.
Li, T., Tian, C., Scalmani, P., Frassoni, C., Mantegazza, M., Wang, Y., et al. (2014). Action potential initiation in neocortical inhibitory interneurons. PLoS Biol, 12, e1001944.
Arellano, J. I., Munoz, A., Ballesteros-Yanez, I., Sola, R. G., DeFelipe, J. (2004). Histopathology and reorganization of chandelier cells in the human epileptic sclerotic hippocampus. Brain, 127(1), 45-64.
[+] Other Work By Ashlynn Dean
Levels of blood proteins within the brain may be linked to major depressive disorder
Neuroanatomy
A new study found that asymmetry of the frontal areas of the brain was positively correlated with thoughts of suicide in patients with Major Depressive Disorder (MDD).
Review of Drug Addiction and the Role of Perineuronal Nets
Neuroscience In Review