Predicting nausea using AI
A new study shows that artificial intelligence may be able to predict an individual's susceptibility to nausea.
Author: Alex Jensen
Download: [ PDF ]
Neuroanatomy
Nausea leaves individuals in pain, feeling weak, with little to no appetite, and often leads to vomiting. There can be several underlying causes for nausea, leaving many suffering from this discomfort.1 Nausea is an adverse feeling that some individuals are more prone to than others. This increased or decreased susceptibility to nausea may contain underlying biomarkers within the brain.2 This study investigates functional and anatomical biomarkers within the brain that may predict nausea susceptibility in individuals. This research is then applied to machine learning to investigate the possibility of computer programs predicting susceptibility or resistance to nausea.3 The resulting model will then be able to assign nausea susceptible or nausea resistant to any individual accurately.
There are many available treatments for nausea but knowing the cause of this nausea is essential. The knowledge of whether or not an individual is prone to nausea due to anatomical or functional differences in the brain allows a doctor to accurately treat nausea in a patient.4 Those susceptible to nausea require different treatment from those with underlying medical causes of nausea.5 Machine learning used to predict nausea susceptibility will let doctors diagnose and treat nausea accurately.
Machine learning allows researchers to use technology to find statistical patterns in data. This use of technology simplifies large sets of data and increases the scope and complexity of problems that can be solved through research.6 A machine can be trained to solve problems and analyze data quicker and easier than humans, broadening the amount of issues that can be solved, including nausea susceptibility.7
28 healthy participants between the ages of 18-65 were used for assessing nausea. In order to induce nausea, participants wore MR-compatible goggles that would project a 10-minute video during an fMRI scan. This video was comprised of still images of a landscape, each tilted and rotated to simulate the perception of spinning about a tilted axis. This was shown to enhance and induce motion sickness. A second MRI was taken while the participants watched a single, still image; this was used as a control. Nausea was assessed using a 4-point visual analogue scale (VAS), where 1 means there are no symptoms of nausea and 4 indicates severe nausea.8 Two questionnaires were also used, the motion sickness sensitivity score (MSSQ) and the motion sickness assessment questionnaire (MSAQ), to assess susceptibility to nausea and symptoms of motion sickness respectively.9
Resting autonomic parameters, including heart rate, were established for the participants before MRIs were taken. Machine learning was used to identify regions of interest within the brain to extract data. Regions identified include the bilateral nucleus accumbens, the amygdala, caudate, hippocampus, pallidum, putamen, and thalamus. The hypothalamus, bilateral insula, bilateral orbitofrontal cortex and anterior (ACC), middle (MCC), and posterior cingulate cortices were also added for additional analysis. Computer programs were then used to identify statistically significant differences within these areas that are contingent on nausea severity, comparing the nausea-induced MRIs to the control MRIs of the participants.
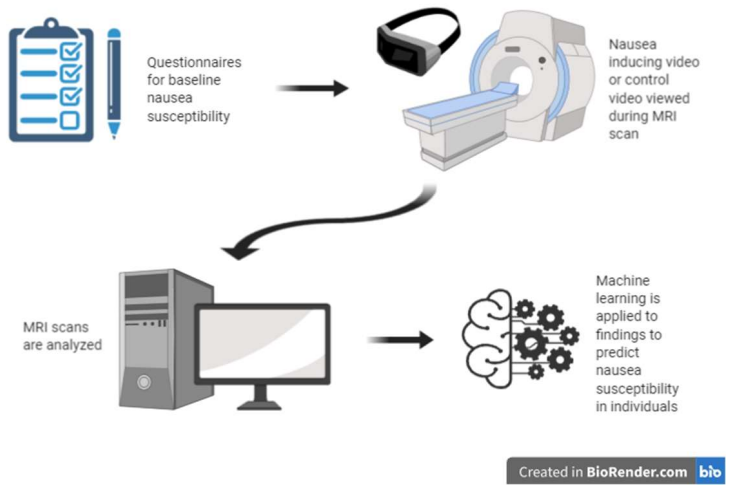
A model was created to predict nausea susceptibility using machine learning. This model was designed as a binary, giving results of either 0 or 1. A 0 indicates nausea resistance in an individual while a 1 indicates nausea susceptibility in an individual. Neuroanatomical features, connectivity features, and autonomic (parasympathetic and sympathetic) features are used to predict nausea susceptibility.10 These steps are summarized in figure 1 below for reference.
From this research, it was found that the MSSQ score was not an effective predictor for nausea sensitivity. The MSSQ score showed no significant correlation with the VAS score or the MSAQ score. This means that, in response to this stimulus, the MSSQ score was a poor predictive measure for nausea severity in the participants. In regard to these results, the VAS score is used as an effective prediction for nausea. The severity of the VAS score during the fMRI showed a significant correlation with sympathetic and parasympathetic activity, showing the ability of VAS to predict an individual’s nausea susceptibility.
The model for machine learning was trained using 70% of the susceptibility data and obtained an accuracy of 80% when predicting nausea susceptibility in this data set. The model was then used to predict nausea susceptibility of the remaining 30% of the data. The model was able to accurately assign nausea susceptibility or resistance to 100% of the individuals in this remaining section of data when compared to the respective individual’s VAS score.
Small anatomical and functional differences in the brain can correspond to struggles in daily life, as seen through susceptibility to nausea. Research in nausea susceptibility is needed in order to fully understand the inner workings of the brain.11 This research uncovers underlying differences that impact an individual’s life and physical comfort by affecting susceptibility to nausea. This will lay the foundation for understanding the causes of nausea susceptibility and resistance.
[+] References
Stanford. (2020). “Chronic Nausea.” Stanford Health Care. https://stanfordhealthcare.org/medical-conditions/digestion-and-metabolic-health/chronic-nausea.html
Singh P., Yoon S. S., & Kuo B. (2016). “Nausea: A Review of Pathophysiology and Therapeutics.” Therapeutic Advances in Gastroenterology, 9 (1), 98.
Horn, C. C. (2008). “Why is The Neurobiology of Nausea and Vomiting so Important?” Appetite, 50 (2-3), 430-434.
Napadow V., Sheehan J. D., Kim J., LaCount L. T., Park K., Kaptchuk T. J., Rosen B. R., & Kuo B. (2012). “The Brain Circuitry Underlying the Temporal Evolution of Nausea in Humans.” Cerebral Cortex, 23 (4), 806-813.
Darvall, J. N. and Leslie, K. (2019). “Pounds of Prevention but Only Ounces of Cure: The Need for More Research on the Treatment of Postoperative Nausea and Vomiting.” Anesthesiology, 130 (2), 183-185.
Branson, K. and Thiels, E. (2019, June 26). “Machine Learning in Neuroscience: Fundamentals and Possibilities.” Neuronline. https://neuronline.sfn.org/scientific-research/machine-learning-in-neuroscience-fundamentals-and-possibilities
Swift, J. (2019). “How we Use Machine Learning.” Cornel Research. https://research.cornell.edu/news-features/howwe-use-machine-learning
Promes S. B., Hendey G.W., & Emerg A. (2005). “Measuring Nausea on a Visual-Analog Scale.” New England Journal of Medicine, 45 (1), 77-81.
Gianaros P. J., Muth E. R., Mordkoff J. T., Levine M. E., & Stern R. M. (2001). “A Questionnaire for the Assessment of the Multiple Dimensions of Motion Sickness.” Aviation, Space, and Environmental Medicine, 72 (2), 115-119.
Ruffle J. K., Patel A., Giampietro V., Howard M. A., Sanger G. J., Andrews P. L. R., Williams S. C. R, Aziz Q., & Farmer A. D. (2019). “Functional Brain Networks and Neuroanatomy Underpinning Nausea Severity Can Predict Nausea Susceptibility Using Machine Learning.” The Journal of Physiology, 597 (6), 1517-1529.
Golding, J. F. (2006). “Motion Sickness Susceptibility.” Autonomic Neuroscience Basic & Clinical, 129 (1-2), 67-76
[+] Other Work By Alex Jensen
Amyloid-β induces pyroptotic neuronal death in Alzheimer’s Disease
Neuroscience In Review
Impact of Air Pollution on the Brain
Neurophysiology
Exposure to diesel exhaust particles causes neuroinflammation, impaired memory, and anxious behaviour in mice.