A PHENOMenal Study Unravels the Mysteries of Schizophrenia
A new study across three countries reveals two distinct subtypes of schizophrenia may exist. Only time can tell how this will affect future treatment protocols!
Author: Kaylee Coats
Neuroanatomy
Introduction
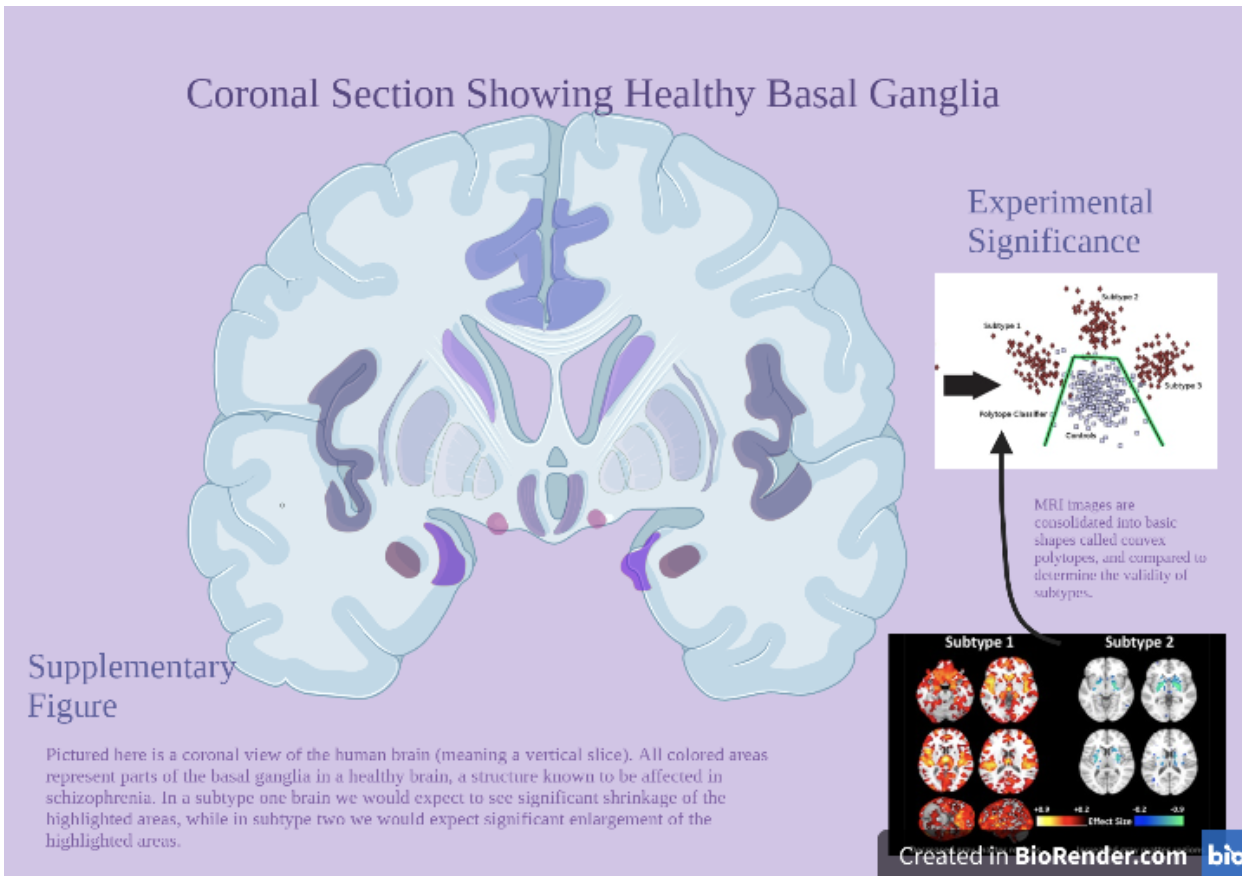
Schizophrenia is a mental health disorder characterized by delusional beliefs, hallucinations, and severe impacts on social functioning. Considering the devastating effects this disorder can have on a person’s life and the lives of those close to them, it is no wonder that scientists want to know more about what it does to the brain. In previous research studies it has been discovered that many schizophrenic patients seem to have “smaller” brains than healthy individuals, particularly in areas of the brain related to emotional and memory regulation such as the hippocampus, thalamus, and basal ganglia. However, up to this point no anatomical subtypes have been defined to better inform treatment protocols. In a new study published in the journal ‘Brain’ by Busatto, Chand, Crespo-Facorro and colleagues, new research techniques were used to solve just this problem. Called Psychosis Heterogeneity Evaluated via Dimensional Neuroimaging (PHENOM) and Heterogeneity through Discriminative Analysis (HYDRA), detailed images were taken of both diseased and healthy brains. These images covered individual brain areas and were then combined into detailed composite images. Researchers concluded that while changing brain volume is characteristic of schizophrenia, there are more specific subtypes to those changes than previously thought. In one subtype, patients are characterized by distinct loss of brain volume and worse functional outcomes, while in subtype two patients are characterized by enlargement of certain brain structures and better functional outcomes. The results of this study tell us that there is more variation among schizophrenia patients than previously thought, and this could inform more effective treatment protocols in the future.
Background
Prior research into the possibility of identifiable biomarkers for mental health disorders such as schizophrenia, and thus biological subtypes, has largely focused on biochemical or genetic differences versus neuroanatomical differences. For example, a 2019 study of postmortem healthy versus schizophrenic brains found differences in the properties of brain proteins (Gleason, Lee, & MacDonald et.al. 2019). It was proposed that these differences may affect the ability of patients’ brains to receive and transmit signals properly within certain structures (2019). Another study used fMRI imaging to track brain activity in schizophrenic brains versus healthy controls (Argylean, Buchanan, & Calarco et.al. 2019). Again, while differences in activation and possible subtypes related to this were found, it was not concluded that those types present differently in clinical practice, nor did it inform further treatment protocols (2019). MRI has been used to identify some neuroanatomical differences among mental health disorders, including schizophrenia. These studies have largely identified thickness of the brain tissue as possible indicators of mental illness, but again this does not directly correlate with the presentation of the illness or possible treatments (Abe, Aoki, & Gonoi et.al. 2020).
Methods
PHENOM is a method of classifying mental health biomarkers using fMRI (a special type of MRI which measures brain activity) and data mapping (Ameis, Jacobs, & Voineskos, 2019). The research so far has concluded that there simply are not black and white neuroanatomical definitions for most mental health disorders, so it instead aims to create a generalized image of the differences seen in healthy versus unhealthy brains (2019). For example, a study on schizophrenia such as this one may focus fMRI images on the hippocampus or basal ganglia. In this study PHENOM was the method of data collection, while HYDRA processed the data. Three subgroups of healthy and unhealthy individuals were used (German, Chinese, and US), with images being obtained from fMRI or MRI imaging as available in each sampling area (Busatto, Chand, & Crespo-Facorro et.al., 2020). This is known as a multiethnic cohort study, meaning that multiple ethnic groups were used in sampling data (Altshuler, Henderson, & Kolonel, 2004). HYDRA is a method of clustering MRI data for illness specific differences by reducing the images to basic geometric shapes called convex polytopes and measuring those shapes (Davatsikos, Sotiras, & Varol, 2016). An algorithm specific to HYDRA is then used to identify patterns, and thus subtypes, within the data (Davatsikos, Sotiras, & Varol, Feb. 2016).
Results
Data analysis revealed two distinct subtypes represented by the samples. In the first subtype there was a specific pattern of gray matter reduction, largely in the thalamus, basal ganglia, and some regions of cortex (Busatto, Chand, & Crespo-Facorro et.al. 2020). The severity of these reductions was further linked to a longer duration of illness (2020). Widespread white matter reduction also occurs in this subtype, as well as an average of lower educational attainment (2020). In subtype two the brain anatomy is mostly normal, minus some enlargements of gray matter in the basal ganglia and innermost white matter (2020). This subtype sees higher educational attainment than subtype one and has no links to illness duration (2020).
Conclusion
While previous MRI studies have been unable to distinguish specific subtypes of schizophrenia due to the overlap of blatant anatomical differences, this study gives the first clinical presentation of potentially clear-cut subtypes. This means that with future research in this area, care for these patients could be made more precise. For example, in another connection to a previous study it has been found that the brains of infants with genetic predisposition to schizophrenia also have observable differences, namely that male infants seem to have enlarged structures while the females show no such differences (Evans, Gerig, & Gilmore et.al., 2010). In subtype two identified here there is enlargement of some structures. It is possible that with further study these genetic markers could also be tied to neuroanatomical differences. Additionally, future research could investigate specific areas of volume reduction or enlargement to further inform treatments. For example, modest decreases in hippocampal volume have been tied to schizophrenia (Eleiz, Sandini, & Schaer, 2019). Further research suggests a link between hippocampal atrophy in adolescence and emergence of positive psychotic symptoms (Anand & Dhikav, 2012). If further analysis of affected areas such as the thalamus and basal ganglia are conducted, this could lead to recognition of additional factors in the onset of disease. Overall, this article was not only fascinating, but it spoke of hope for future sufferers of what can be a debilitating mental health disorder.
[+] References
Abe, O., Aoki, Y., Gonoi, W., Iwashiro, N., & Kasai, K. et. al. (Aug. 17th, 2020). Machine-learning classification using neuroimaging data in schizophrenia, autism, ultra-high risk and first episode psychosis. Translational Psychiatry. Aug.; 278(10): n.p.
Altshuler, D., Henderson, B.E., & Kolonel, L.N. (July 1st, 2004). The multiethnic cohort study: exploring genes, lifestyle and cancer risk. Nature Reviews Cancer. July; 4: 519-527.
Ameis, S.H., Jacobs, G.R., & Voineskos, A.N. (Sept. 17th, 2019). Neuroimaging Heterogeneity in Psychosis: Neurobiological Underpinnings and Opportunities for Prognostic and Therapeutic Innovation. Biol Psychiatry. July; 88(1):95-102.
Anand, K.S., & V. Dhikav. (Oct-Dec 2012). Hippocampus in health and disease: An overview. Annals of Indian Academy of Neurlogy. Oct-Dec; 15(4):239-246.
Argyelan, M., Buchanan, R.W., Calarco, N., DeRosse, P., & Dickie, E.W. et.al. (Jan. 4th 2019). Separable and Replicable Neural Strategies During Social Brain Function in People With and Without Severe Mental Illness. The American Journal of Psychiatry. July; 176(7):521-530.
Busatto, G.S., Chand, G.B., Crespo-Facorro, B., Davatzikos, C., & Dazzan, P. et.al. (March 2020). Two distinct neuroanatomical subtypes of schizophrenia revealed using machine learning. Brain: A Journal of Neurlogy. March; 143(3):1027-1038.
Davatsikos, C., Sotiras, A., & Varol, E. (2016). HYDRA: Heterogeneity through Discriminative Analysis [Article]. Retrieved from https://www.med.upenn.edu/cbica/sbia/hydra.html.
Davatsikos, C., Sotiras, A., & Varol, E. (Feb. 23rd, 2016). HYDRA: Revealing Heterogeneity of imaging and genetic patterns through a multiple max-margin Discriminative Analysis framework. Neuroimage. Jan. 15th 2017; 145(15ptB): 346-364.
Eleiz, S., Mancini, V., Sandini, C., Schaer, M., & Schneider, M. et.al. (June 4th, 2019). Positive psychotic symptoms are associated with divergent developmental trajectories of hippocampal volume during late adolescence in patients with 22q11DS. Molecular Psychiatry. Nov. 2020; 25:2844-2859.
Evans, D.D., Gerig, G., Gilmore J.H., Hamer, R.M., & Kang, C. et.al. (Sept. 1st, 2010). Prenatal and Neonatal Brain Structure and White Matter Maturation in Children at High Risk for Schizophrenia. The American Journal of Psychiatry. Sept; 167(9): 1083-1091.
Gleason, K., Lee, B.J., MacDonald, M.L., Margolis, R.L., & Nucifora Jr, F.C. et. al. (May 6th 2019). Increased Protein Insolubility in Brains From a Subset of Patients With Schizophrenia. The American Journal of Psychiatry. Sept.; 176(9):730-743.