Scientists Figure Out How to Restore Mobility to Paralysis Patients in as Little as One Day
A group of scientists have figured out how to help people with spinal cord injury walk after experiencing complete paralysis, and here’s how they did it.
Author: Timi Mason
Neuroanatomy
An article was published in the February 2022 volume of Nature Medicine, in which a large group of researchers worked together to find a new and more efficient way to help people with lower body paralysis due to spinal cord injury (SCI) walk again. SCI can cause many complications, up to and including paralysis in one or both legs (Disabled World, 2022). The experiment that was laid out and conducted in this article focused on finding a way to help patients walk, stand and conduct other physical activities involving leg movements, such as cycling and swimming. These researchers were able to restore leg and torso movements to their subjects within one day.
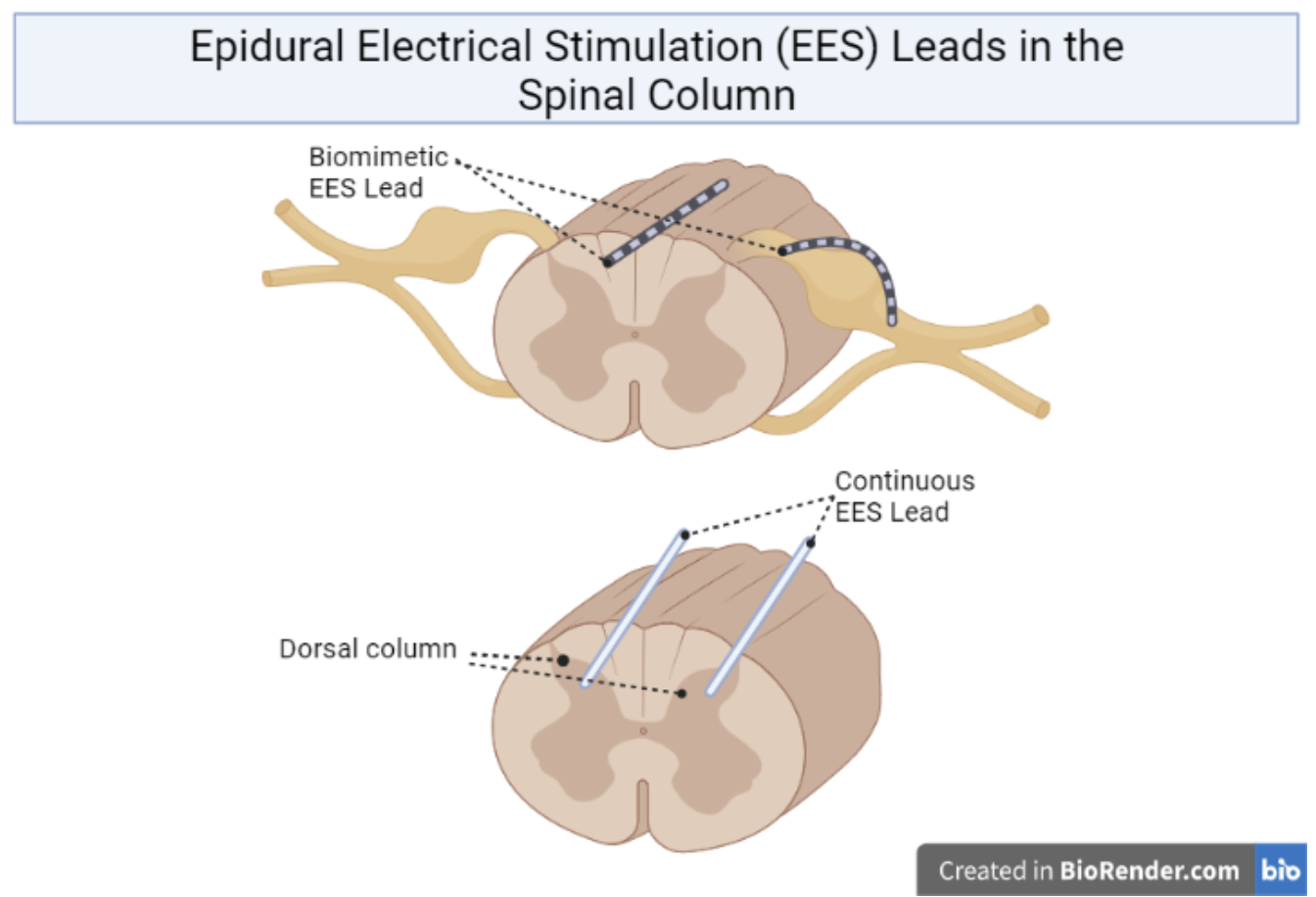
While other methods of treatment exist and are already in practice, this experiment was designed to improve and hasten recovery for patients. Some of the other methods that have been used in the past include medical equipment, prosthetics, and even voice activated technology (Cleveland Clinic, 2021). These methods are meant to improve function and accommodate the patient; they are not meant to aid in healing a spinal cord injury. Continuous epidural electrical stimulation, or EES for short, is a method that has been used in the past to heal SCI (Formento, et al., 2018). These kinds of experiments showed results after months of therapy (Rowald et al., 2022). Rowald and associates worked to fine tune this method, using biomimetic EES – they used EES in a way that would mimic the body’s biological processes.
The target for continuous EES is the dorsal (rear) side of the spinal column, whereas the biomimetic EES targets the dorsal roots of the spinal column – a much more specific site than the former method uses (Rowald et al., 2022). This is illustrated in Figure 1 below. Rowald and associates designed the paddle leads and the software that connects the electronics together.
The researchers realized quickly that there is a lot of variation in spinal length and spacing in the human population. Spinal length differs from person to person depending on their height; the average length of the spine for males is 71 centimeters, and 61 centimeters for females (Kayalioglu, 2008). Rowald and associates stated in their article that because of this, a wider use of their technology would require either a large catalog of differently sized paddle leads or personalized paddle leads for each individual patient. Personalized medical apparatuses are not a new concept; people must be fitted for dentures and prosthetics, for instance, in order to use them.
Rowald and associates first performed their experiment in simulation before moving on to live subjects. Once they were able to predict where to place the leads, the live subject had an intraoperative 3-D Ct scan done, and then placement of the electrodes. They did test if alternative placement locations would work, but found that the predicted locations yielded the best results (Rowald et al., 2022). According to their paper, all three of the subjects for this study were able to walk independently on a treadmill within the first day, but with unnatural gait. The subjects were able to walk with a slightly steadier gait while supported within 1 to 3 days after the initial day. Each of the 3 subjects went through a 5 month program for rehabilitation, which resulted in them being able to bear their own weight and stand/walk independently with the assistance of a walker (Rowald et al., 2022).
The participants did not gain an entirely steady gait by the end of the experiment, but they were able to walk and perform activities such as standing for extended periods and riding a recumbent bike (Rowald et al., 2022). This is an improvement from past experiments, such as in the case of Formento et al. This has possibly opened a pathway to even more significant advances in this field, and aided to give us a better understanding of how the spinal column, and especially the dorsal roots, play a part in our ability to carry out every day tasks.
[+] References
Cleveland Clinic (2022, June 10). Paralysis: What is it, Diagnosis, Management & Prevention. https://my.clevelandclinic.org/health/diseases/15345-paralysis#management-and-treatment
Disabled World (2017, December 1). Human Spine and Spinal Cord C1 to S5 Vertebra. (Updated 2022, April 14). https://www.disabled-world.com/disability/types/spinal/spine-picture.php#:~:text=The%20human%20spinal%20cord%2C%20part,thick%20in%20the%20thoracic%20area.
Formento, E., Minassian, K. et al. (2018) Electrical spinal cord stimulation must preserve proprioception to enable locomotion in humans with spinal cord injury. Nat Neurosci. 21 (12): 1728–41. https://doi.org/10.1038/s41593-018-0262-6
Kayalioglu, G. (2008). The Spinal Cord. Elsevier Ltd. Retrieved from https://doi.org/10.1016/C2009-0-01677-8
Rowald, A., Komi, S., Demesmaeker, R. et al. (2022) Activity-dependent spinal cord neuromodulation rapidly restores trunk and leg motor functions after complete paralysis. Nat Med 28, 260–271. https://doi.org/10.1038/s41591-021-01663-5