Are We Excited Yet? The Autistic Brain May Experience Heightened Excitation Due to Fewer Chandelier Cells
A new study from UC Davis suggests that autistic traits may be partially due to decreased numbers of silencing cells
Author: Rachel Buzzelle
Neurophysiology
Despite first being described at the dawn of the 20th century, autism was not nearly as hot a topic until the publication of Andrew Wakefield’s discredited paper linking the condition to the MMR vaccine. Consequently, media reporting on autism research has focused on the investigation between this purported link to reassure the public of vaccination’s safety. However, this is only one of many avenues of research being conducted into the condition. Last year, a team led by Dr. Sarwat Amina verified and quantified a decreased expression of chandelier cells in people diagnosed with autism. The findings support a long-standing hypothesis that autistic traits may be due to altered states of excitation as compared to neurotypical brains. Autism activists often justifiably balk when their condition is referred to as a disease in need of treatment, and this is a position to which researchers need to be sensitive. However, unravelling the neural roots of autism has the potential to alleviate the struggles of people living with its most severe forms and contributes to the wider body of knowledge surrounding the implications of cellular and circuit diversity.
Background
The catch-all term autism refers to a spectrum of disorders characterized by altered social communication and behavior; repetitive behaviors; and niche, obsessive interests. The impact autism has on the individual varies wildly: The majority are just as capable at living independent lives as their non-autistic peers. Unfortunately, those not included in that number often have severe developmental delays that impede their ability to care for themselves.vi Autistic people also tend to share other similarities such as unusual sleeping habits, gastrointestinal issues, seizure disorders, and comorbid neuropsychological disorders.v This interplay between brain and body is partially why researchers are so interested in puzzling out the physiological origins of autism.
Scientists in the field have suspected since at least the late 90’s that altered excitation and inhibition patterns of specific sensory, memory, social, and emotional circuits could underlie the expression of autism. Less clear was how the activity of nerve circuits was being altered. The observed excitation could be explained through changes in cell populations, changes in the circuitry itself, or both.iii As a starting point, interneurons posed a particularly tantalizing target as they function as neuronal “brakes” to decrease and synchronize activity in the integrative areas of the brain. In previous experimentation, the UC Davis lab had determined that of the 3 general classes of inhibitory interneuron, only parvalbumin-positive (PV+) ones were decreased in autism. The lab then followed up with a second study to determine the extent of reduction in PV+ cell types and found that the reduction occurred almost entirely in chandelier cells (ChCs) as opposed to basket cells.
ChCs are striking structures. A subclass of inhibitory interneurons, their axons end in many branching terminals called cartridges.iii Each cartridge terminates in one or more boutons that can synapse with the axon initial segment of excitatory pyramidal cells (ePCs).iii While each ePC may only be innervated by 1 – 3 ChCs, the ChCs are capable of innervating many ePCs.iii Through these many connections, populations of ChCs can selectively calm the activity of ePCs and synchronize their activity.iii Based on the excitation/inhibition imbalance theory of autism, and armed with the results of their previous work, the team then set out to determine if ChCs themselves are reduced in the autistic brain or if the cartridges are present, but not expressing PV.
Methods
The team acquired postmortem samples of brain tissue from eleven autistic individuals and eleven control individuals via the Autism Tissue Program.iii For this study, a control subject was defined as not having any neurological disorder based on medical records and information from next of kin.iii The subjects ranged in age from 7 to 24 years old at the time of death and represented a variety of causes of death.iii Tissue samples were taken from the Broadman areas (BA) 9, 46, and 47.iii These regions were chosen because they represented areas of the brain that are spatially distinct. Each sample was thinly cut by a cryostat and a small portion was Nissl stained to positively identify the cortex of origin.iii Areas surrounding the Nissl stain were then immunostained with antibodies for GABA transporter 1 protein (GAT1), a known label for ChC cartridges.iii After staining, the researchers examined a 3mm bin encompassing all cortical layers and counted the number of cartridges present.iii This process was replicated once more on a different tissue sample for each cortical area.iii Since the goal of the study was to determine if there is a significant difference in the number of ChCs found in autistic versus control brains, the results were analyzed with a t-test.iii The researchers also attempted to account for other factors such as age at death and time in storage using ANOVA.iii
Results
The researchers found that autistic brains did indeed express fewer ChCs in all areas sampled when compared to the cell populations of controls.iii The reduction was moderate and roughly equivalent in BA9 and BA47, but BA46 exhibited a dramatic decrease in ChC populations at a 61% reduction.iii Most interestingly, these results aligned quite nicely with the data from the study that aimed to quantify the reduction in PV+ interneurons. For BA9, the loss of PV+ interneurons was found to be 42% and the reduction in cartridges was 39%.iii In BA46, there was a 60% decrease in PV+ soma and a 61% decrease in cartridges.iii Finally, in BA47, PV+ soma were reduced by 31% and cartridges were reduced by 46% in autistic samples.iii The authors did note that the slight differences between the studies could be due to the influence of age.iii The older study used a larger age range of samples and ChC density changes with age.iii Though the researchers attempted to account for any confounding factors via ANOVA, none of the analyses returned any significant findings.iii
Significance
Not only was the UC Davis team able to determine that the reduction in PV+ interneurons seen in earlier work was due to a reduction of ChC cartridges, they also validated the findings of those studies by reporting similar results. Since the percent decreases in PV+ interneurons and ChCs
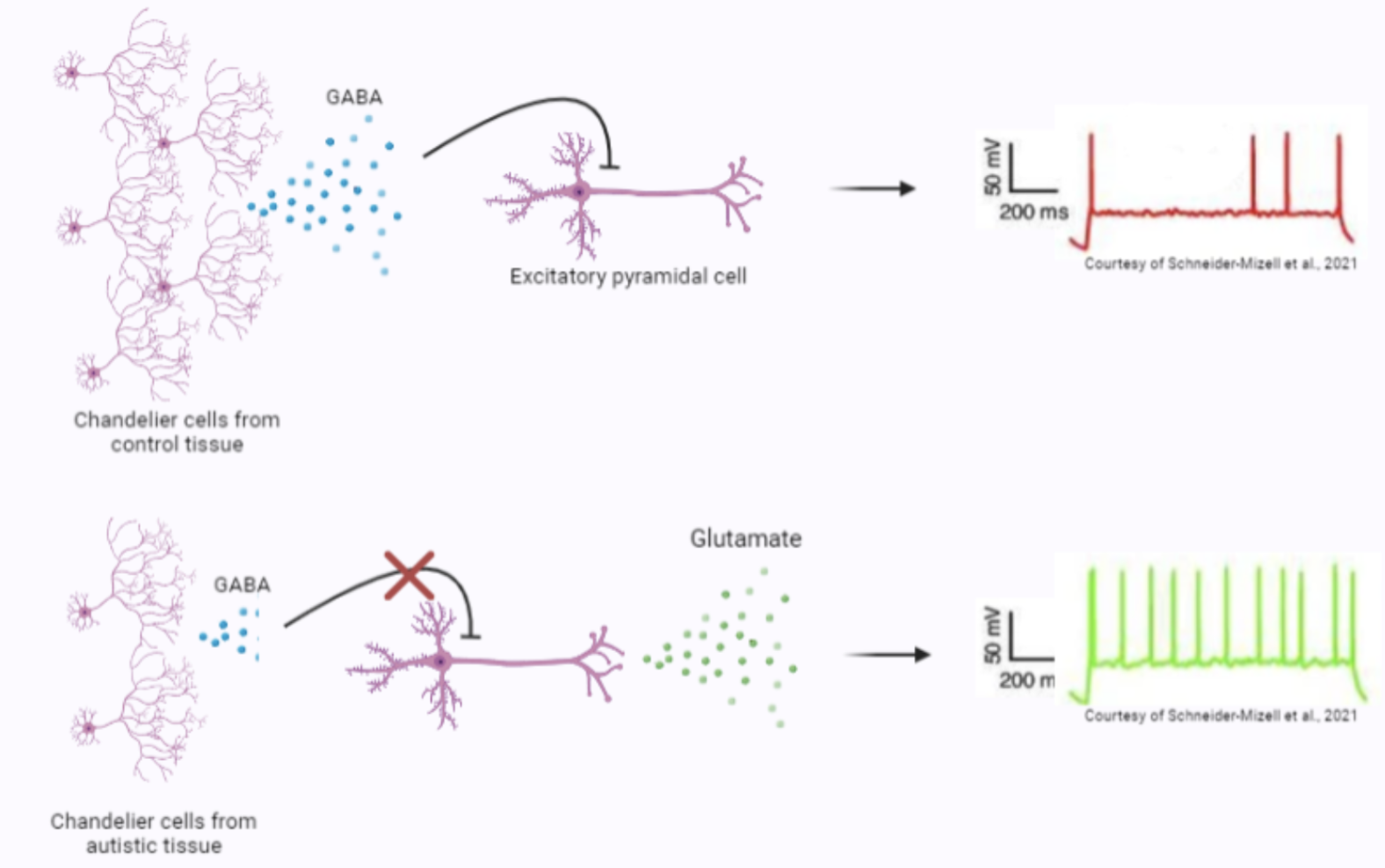
are so similar, it does strongly suggest that the dearth of PV+ soma is sufficiently explained by a loss of ChCs. This implies that the excitation/inhibition imbalance seen in autism is primarily caused by an increase of excitation in key cortical areas. Since ChCs are powerful inhibitors of excitatory neurons, their absence most likely leads to greater excitation states than one might expect in a neurotypical brain. As seen in figure 1, fewer ChCs release less GABA. They may release so little that ePCs are not inhibited and continue to elicit excitation through glutamate release. The authors are careful to note that they have not yet ascertained if the ChCs in autistic people are compensating in some way to make up for being fewer in number.iii More research is needed, and next steps should include accounting for cellular adaptations that could augment the inhibitory power of ChCs such as an increased number of synaptic boutons, an increase in the number of vesicles released or the amount of GABA in each vesicle, and overall activity level of the ChCs. These could be investigated through genetic fluorescent labeling, electrophysiological, and biochemical investigations.,
Researchers must be cautious not to over-pathologize people with autism. Many with the condition consider it a key part of their identity and do not wish for “treatment”.iv We must also not discount the value of diverse perspectives from neurodivergent individuals – one must look no further than the contributions made by visionaries such as scientist Temple Grandin and jazz musician Matt Savage. However, some forms are autism are much more severe than others and can pose hardships on the individual and their family. Unearthing the mechanism of autism at scale could help lead to interventions, pharmaceutical and otherwise, that increase the quality of life for such people. Those with milder
forms of autism may also benefit if such discoveries explain some of the inconvenient comorbidities that can
accompany autism. In any case, this study serves to reminds us of the beauty of neurological variation and how our
perception of the world itself begins in our cells.
[+] References
Godlee, F., Smith, J., & Marcovitch, H. (2011). Wakefield’s article linking MMR vaccine and autism was fraudulent. BMJ, 342(jan05 1), c7452–c7452. https://doi.org/10.1136/bmj.c7452
Davidson, M. (2017). Vaccination as a cause of autism—myths and controversies. Dialogues in Clinical Neuroscience, 19(4), 403–407. https://doi.org/10.31887/dcns.2017.19.4/mdavidson
Amina, S., Falcone, C., Hong, T., Wolf-Ochoa, M. W., Vakilzadeh, G., Allen, E., Perez-Castro, R., Kargar, M., Noctor, S., & Martínez-Cerdeño, V. (2021). Chandelier Cartridge Density Is Reduced in the Prefrontal Cortex in Autism. Cerebral Cortex, 31(6), 2944–2951. https://doi.org/10.1093/cercor/bhaa402
Sherwood, H. (2021, June 27). “We don’t need to be cured or fixed”: writers speak out on autism. The Guardian; The Guardian. https://www.theguardian.com/society/2021/jun/27/we-dont-need-to-be-cured-or-fixed-writers-speak-out-on-autism
CDC. (2022, March 28). Signs and Symptoms of Autism Spectrum Disorders. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/autism/signs.html
Wolff, N., Stroth, S., Kamp-Becker, I., Roepke, S., & Roessner, V. (2022). Autism Spectrum Disorder and IQ – A Complex Interplay. Frontiers in Psychiatry, 13. https://doi.org/10.3389/fpsyt.2022.856084
Lee, E., Lee, J., & Kim, E. (2017). Excitation/Inhibition Imbalance in Animal Models of Autism Spectrum Disorders. Biological Psychiatry, 81(10), 838–847. https://doi.org/10.1016/j.biopsych.2016.05.011
Hashemi, E., Ariza, J., Rogers, H., Noctor, S. C., & Martínez-Cerdeño, V. (2016). The Number of Parvalbumin-Expressing Interneurons Is Decreased in the Medial Prefrontal Cortex in Autism. Cerebral Cortex, bhw021. https://doi.org/10.1093/cercor/bhw02
Ariza, J., Rogers, H., Hashemi, E., Noctor, S. C., & Martínez-Cerdeño, V. (2016). The Number of Chandelier and Basket Cells Are Differentially Decreased in Prefrontal Cortex in Autism. Cerebral Cortex, 28(2), 411–420. https://doi.org/10.1093/cercor/bhw349
Wang, Y., Zhang, P., & Wyskiel, D. R. (2016). Chandelier Cells in Functional and Dysfunctional Neural Circuits. Frontiers in Neural Circuits, 10. https://doi.org/10.3389/fncir.2016.00033
Lees, R. M., Johnson, J. D., & Ashby, M. C. (2020). Presynaptic Boutons That Contain Mitochondria Are More Stable. Frontiers in Synaptic Neuroscience, 11. https://doi.org/10.3389/fnsyn.2019.00037
Povysheva, N. V., Zaitsev, A. V., Gonzalez-Burgos, G., & Lewis, D. A. (2013). Electrophysiological Heterogeneity of Fast-Spiking Interneurons: Chandelier versus Basket Cells. PLoS ONE, 8(8), e70553. https://doi.org/10.1371/journal.pone.0070553
[+] Other Work By Rachel Buzzelle
Detangling Prion Disease: Promising Research Hints at Future Treatments
Neuroanatomy
Prion infected nervous tissue treated with resveratrol experienced both the eradication of disease and amelioration of the recovering tissue’s microenvironment.