The key to an effective anti-depressant regiment: brain-derived neurotrophic factor
Author: Jonah Stickney
Download: [ PDF ]
Neuroanatomy
Major depressive disorder is hyper-prevalent in today’s society. The National Institute of Mental Health estimates that 17.3 million adults in the United States have had at least one major depressive episode, 7.1% of all adults (NIMH, 2019). There are significant symptoms of MDD that may impede the lives of those living with it; reduced motivation, severe changes in diet and sleep, and in some, suicidal ideation. Part of the tenacity of MDD is the ability for these symptoms to further exacerbate the negative affect caused by depression in a positive feedback loop. If we better understood how to effectively treat these symptoms, it may improve the treatment outcomes of millions. One of these symptoms that is not fully understood is memory disruption. In recent study published in 2019 and performed by German scientists, brain derived neurotropic factor (BDNF) was correlated with the memory restoration in MDD patients being treated with antidepressants.1 Understanding this correlation, BDNF levels could be used as a measure of antidepressant efficacy in patients who have impaired memory. Exogenous BDNF could also prove to be a novel treatment to treat memory impairment.
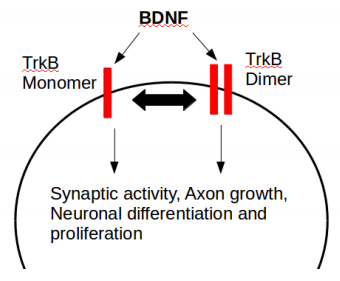
BDNF serum, blood and hair levels have recently been used in many research projects as a measure for the severity of various multiple disorders (especially depression, chronic stress and psychosis spectrum disorders). Measured thusly, BDNF seems to be an antagonist to cortisol when it comes to mental health prognosis.2 Why is there so much focus on measuring this specific neurotrophin as opposed to nerve growth factor or neurotrophins 3 and 4? In healthy individuals, BDNF has widespread expression both within and outside of the central nervous system. On a microscopic level, BDNF is a potent regulator for synaptic plasticity via LTP, especially within the hippocampus. BDNF acts on the tyrosine kinase B receptor (TrkB) so serum BDNF is often measured alongside level of TrkB expression (Figure 1).3 BDNF levels alter neurotransmitter release, glutamate receptor density, protein synthesis and structural plasticity at dendritic spines which sum to affect on learning and memory.3 If this is the local effect of BDNF, what is its global effect? This is the topic of interest for the research project of discussion.
The study of interest was an investigation into a large clinical trial (n=173) aiming to improve depression treatment: is there a significant difference in outcome between groups who receive early medication change (EMC) and those who receive treatment as usual (TAU). Antidepressants have a slow clinical onset and therefore treatment as usual consists of waiting three weeks before determining whether changing antidepressant dosage or prescription is appropriate. Early medication change as a treatment is defined by changing antidepressant (escitalopram to venlafaxine) in non-responding patients after only 2 weeks. A battery of memory tests known collectively as the Verbal Learning and Memory Test (VLMT) were performed three times during the experiment; at baseline, day 28 and day 56. Blood was drawn to measure plasma BDNF levels at baseline, day 14 and day 56. Depression level was monitored throughout using the Hamilton Depression Rating Scale (HAMD). ANCOVAs were performed between HAMD scores and learning and delayed recall, corrected for age, IQ and sex. Memory performance and plasma BDNF (pBDNF) was compared using repeated measures ANOVAs. Significance level was set at an alpha of 0.05.
Learning performance improved for the group regardless of treatment but this may be due to increased familiarity to the memory test. Most comparisons made statistically with BDNF in this project were found to be non-significant. Depression severity was not correlated with memory or learning performance. Similarly, plasma BDNF and memory performance were not correlated. In fact, in a different study BDNF serum levels did not differ between those with and without depression (Dols et al., 2015). There was one group in this experiment that did show significance. In the sample, 36% of patients showed memory deficits at baseline, 24% had impaired learning and 32% had delayed recall of word lists. Approximately 40% of these patients had memory normalization during the course of the experiment. In this subgroup of patients (those who initially had memory impairments and recovered), pBDNF and normalization of memory were significant when compared to those with persistent impairments. It is important to note that this significance is not an increase of BDNF during the experiment but rather a higher BDNF at baseline that was significant in predicting whether a patient would have normalization of memory (Average pBDNF was 1218.5 ug/ml for the normalization group and 769.1 ug/ml for the persistent impairment group). This implies that BDNF possibly predisposes anti-depressants to normalize impaired memory.
There is a study similar to this one in which BDNF was measured during an Electro-convulsive therapy of treatment resistant depression. BDNF was measured before and after ECT treatment and was compared to depression score also measured by the Hamilton Depression Rating Scale. In addition, the intensity of the induced seizure was measured by the Seizure Quality Index (SQI). Interestingly, as with the main study of interest, BDNF did not correlate significantly with many factors, including initial and final HAMD scores, age, or rate of remission. Similar to the previous study however there was significance between BDNF and an indirect measure of remission rather than the actual outcome itself; BDNF and SQI score were significantly correlated similar to the correlation between BDNF and memory normalization.4
The relationship between depression and memory functioning is highly elusive. Some studies have shown that memory problems often persist after remission of depression, while others show improvement of memory from a successful antidepressant treatment5 (Heinz et al., 2012). The previous studies support this. Perhaps this is due to depression’s etiology not being understood mechanistically, and in fact depression may be an umbrella term for different syndromes with entirely different etiologies. This is not a divisive statement, especially within clinical psychology. For example, Cushing’s syndrome is sometimes misdiagnosed as treatment resistant depression.6 It is possible that in some cases, memory disruption is an exacerbating cause to the depression while in others, depression is co-morbid with memory disruption unrelated to the depression etiology. This theory would explain why BDNF would not correlate with remission of depression across different treatments, but would only correlate with those suffering from a specific form of depression. In this view, BDNF allows for antidepressant treatment to be more effective (as measured by SQI and memory normalization) but in some cases this is not enough to alleviate depression.
Even though BDNF is not the best measure for depression outcomes, it is still an important factor to consider in the mechanism of depression and its treatment. A team in China recently introduced a traditional Chinese anti-depressant named XingPiJieYu into their lab for study. This extract from the herb of the same name greatly increased serum BDNF in rodents exposed to chronic unpredictable stress.7 This is exciting for the future of antidepressant treatment in which XPJY may be co-prescribed with another anti-depressant to increase its efficacy. This is a promising view but it may be too reductive to view the complex hormonal system would function this way. The UK government funded a large clinical trial (n=165) to see if co-prescribing antiglucocorticoids with antidepressants could better treat depression because chronically elevated cortisol is a common symptom of depression. Unfortunately the study found this co-prescription had no effect on outcome.8 Will BDNF treatment follow the same pattern or will XPJY cause a revolution in depression treatment?
While we wait for clinical trials, what can we do to increase our BDNF? Exercise. It has been well established that aerobic exercise increases systemic BDNF levels, with one study finding that even a single bout of exercise significantly increases BDNF in rodents.9 Two separate studies in particular have gone one step further and have implicated this interaction to be able to predict memory performance, one in rats and the other in young adult humans.10,11 Understanding hormonal systems is vital to develop better clinical therapies.
[+] References
Engelmann J, Wagner S, Wollschlager D, Kaaden S, Schlicht KF, Dreimuller N, Braus DF, Muller MB, Tuscher O, Frieling H, Tadic A, Lieb K. (2019). Higher BDNF plasma levels are associated with a normalization of memory dysfunctions during an antidepressant treatment. European Archives of Psychiatry and Clinical Neuroscience. Mar 30 [Epub ahead of print]
Linz R, Puhlmann LMC, Apostolakou F, Mantzou E, Papassortiriou I, Chrousos GP, Engert V, Singer T. (2019) Acute psychosocial stress increases serum BDNF levels: an antagonistic relation to cortisol but no group differences after mental training. Neuropsychopharmacology. Apr 16 [Epub ahead of print]
Leal G, Bramham CR, Duarte CB. (2017) BDNF and Hippocampal Synaptic Plasticity. Vitamins and Hormones. 104:153-195.
Kranaster L, Hellweg R, Sartorius A. (2019) Association between the novel seizure quality index for the outcome prediction in electroconvulsive therapy and brain-derived neurotrophic factor serum levels. Neuroscience Letters. Apr 9; 704:164-168
Hinkelmann K, Moritz S, Botzenhardt J, Muhtz C, Wiedemann K, Kellner M, Otte C. (2012) Changes in cortisol secretion during antidepressive treatment and cognitive improvement in patients with major depression: A longitudinal study. Psychoneuroendocrinology. May; 37(5):685-692
Anil Kumar BN, Grover S. (2016) Cushing’s Syndrome Masquerading as Treatment Resistant Depression. Indian Journal of Psychological Medicine. May-Jun; 38(3):246-8
Wang C, Guo J, Guo R. (2017) Effect of XingPiJieYu decoction on spatial learning and memory and cAMP-PKACREB-BDNF pathway in rat model of depression through chronic unpredictable stress. BMC Complementary & Alternative Medicine. Jan; 17:73
Ferrier IN, Anderson IM, Barnes J, Gallagher P, Grunze HCR, Haddad PM, House AO, Hughes T, Lloyd AJ, Mamasoula C, McColl E, Pearce S, Siddiqi N, Sinha B, Speed C, steen N, Wainwright J, watson S, Winter FH, McAllister-Williams RH; the ADD Study Team. (2015) Randomised controlled trial of Antiglucocorticoid augmentation (metyrapone) of antiDepressants in Depression (ADD Study). Efficacy and Mechanism Evaluation. Jun.
Venezia AC, Quinlan E, Roth SM. (2017) A single bout of exercise increases hippocampal Bdnf: influence of chronic exercise and noradrenaline. Genes, Brain and Behavior. May 26; 16(8)
Loprinzi PD. (2019) Does brain-derived neurotrophic factor mediate the effects of exercise on memory? The Physician and Sportsmedicine. Apr 19 [Epub ahead of print]
Whiteman AS, Young DE He X, Chen TC, Wagenaar RC, Stern CE, Schon K. (2014) Interaction between serum BDNF and aerobic fitness predicts recognition memory in healthy young adults. Behavioral Brain Research. Feb 1; 259:302-12
Gupta V, You Y, Gupta Veer, Klistorner, Graham S. (2013) TrkB Receptor Signalling: Implications in Neurodegenerative, Psychiatric and Proliferative Disorders. International Hournal of Molecular Sciences. May 13; 14(5):10122-10142
Sorri A, Jarventausta K, Kampman O, Lehtimaki K, Bjorkgvist M, Tuohimaa K, Hamalainen M, Moilanen E, Leinonen E. (2018) Effect of electroconvulsive therapy on brain-derived neurotrophic factor levels in patients with major depressive disorder. Brain and Behavior. Nov; 8(11):ed01101
[+] Other Work By Jonah Stickney
Opioid-induced hyperalgesia and enhanced pain in opioid withdrawal: a comparison of cellular mechanisms
Neuroscience In Review
Want a better memory? More REM sleep could be the solution
Neurophysiology
Sleep has previously been identified as a critical period for consolidation of memory. A research team spanning labs in both New York and Peking recently identified one mechanism that only occurs during one specific stage of sleep: REM sleep. This mechanism is the pruning of dendritic spines.