PTSD and its effects on the amygdala and the anterior cingulate cortex
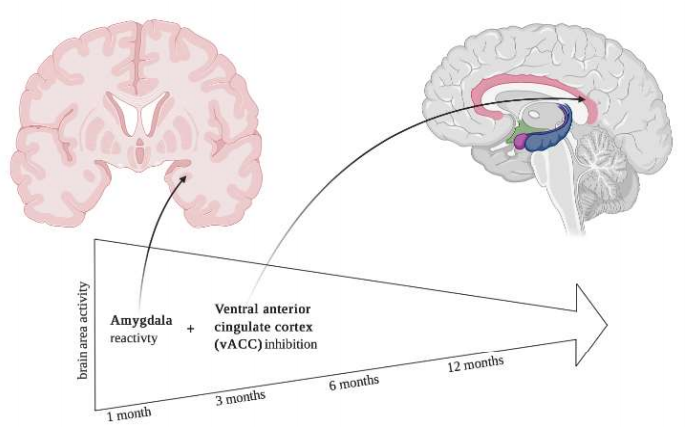
The study aims to show that amygdala hyperactivity following an acute trauma is indicative of chronic post-traumatic stress disorder (PTSD) symptoms. Alternatively, the inability to sustain ventral anterior cingulate cortex activation when being exposed to similar trauma can be linked to difficulty recovering from ongoing PTSD symptoms.
Author: Tori Davis
Download: [ PDF ]
Neuroanatomy
The results of this study work to identify the risk factors that are present in an individual prior to trauma exposure that could potentially predispose them to later developing PTSD. In a paper published in 2017 by Stevens et al., the brain function of individuals who were exposed to a trauma underwent fMRI to analyze the neural reactivity and habituation to fearful and neutral facial stimuli to understand the correlation between the development of PTSD symptoms and amygdala hyperactivity.12 The study showed that there was a strong correlation between the hyperactivity of the dorsal anterior cingulate cortex (dACC) and the amygdala when compared to the symptoms of PTSD. Additionally, the study showed that decreased ventral anterior cingulate cortex (vACC) activity is indicative of more severe PTSD symptoms and difficulty recovering from those symptoms. With this information, providers can work to decrease the activity of the amygdala and/or the dAAC as well as increase the activity of the vACC to help treat PTSD symptoms early before the development of more severe PTSD symptoms.
On average, 50-60% of people are exposed to a trauma in their lifetime, and out of those people, 6-8% end up developing PTSD.1,2 Several studies suggest that connectivity between the amygdala and the dACC is increased when comparing pre-trauma to post trauma as well as when comparing soldiers before going to war and after returning from war.3,4,5 The amygdala can be related to the human response to a fearful stimulus as well as the stress responses to emotional events like trauma that can have an effect on the development of mood disorders like PTSD and depression.6,7 Alternatively, the dACC can be related to cognitive function, learning, and memory as well as arousal, which can function alongside the amygdala.8 By studying these structures and understanding the role they play in individuals with PTSD, the symptoms of these conditions can be minimized before it worsens.
Participants included individuals that had been admitted to an emergency department immediately following a trauma that classified as a criterion A trauma per the DSM-IV-TR and had occurred within the past 24 hours.9 Prior to the study and at the 1-, 2-, 3-, 6-, and 12-month marks, PTSD and depression symptoms were assessed using the PTSD Symptom Scale and the Beck Depression Inventory respectively.10,11 Three weeks following the initial trauma, the participants underwent fMRI imaging to view the amygdala, dACC, and vAAC when viewing randomly alternating 15 fearful and 15 neutral faces. Reactivity was measured by comparing fearful vs. neutral faces using a random effect analysis, and habituation was measured by comparing the first third of the fearful and neutral faces (5 faces) to the last third (5 faces) of the fearful and neutral faces.
The results found that not only are the symptoms of PTSD and depression associated with the hyperactivity of the amygdala, but they are also associated with brain areas that regulate the amygdala’s activity like the vACC, which ultimately is the cause of the amygdala’s hyperactivity. PTSD symptom severity was reassessed 1 month after the initial trauma, which was when the severity was at its worst, and then there was a steady decline by the end of 12 months. However, the symptoms were will moderately present and important to note.
Other findings indicated that the increased amygdala reactivity was present early on following the trauma alongside increased reactivity of the dACC and decreased reactivity of the vACC. The more time passed, the less prevalent the increased reactivity of the dACC and the decreased reactivity of the vACC was noticed. Additionally, there was no effect regarding amygdala habituation, however habituation of the vACC did indicate a worsened recovery time over a 12-month period. This finding is only significant for fearful stimuli. Regardless, overall the data did show that higher amygdala reactivity immediately post-trauma indicates a higher level of PTSD symptom severity after 12 months, and these individuals tended to maintain their PTSD symptoms for a longer period of time in comparison to their counterpart.
In conclusion, this data is important, because it can help providers treat neurological differences in those predisposed to PTSD symptoms and depression immediately following the trauma to help reduce long-term symptoms. Due to the data that showed that the following changes were observed only immediately following the trauma, these negative symptoms can be reduced by treating the increased amygdala reactivity, the increased dACC reactivity, and the decreased vACC reactivity early on after the trauma occurs. This is life-changing news since soldiers and trauma victims in the ED can be treated within three weeks of the exposure and can potentially show less long-term effects, resulting in a higher quality of life for those affected.
[+] References
Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Posttraumatic stress disorder in the National Comorbidity Surgery. Archives of General Psychiatry, 52, 1048–1060.
Stevens, J. S., Kim, Y. J., Galatzer-Levy, I. R., Reddy, R., Ely, T. D., Nemeroff, C. B., … Ressler, K. J. (2017). Amygdala Reactivity and Anterior Cingulate Habituation Predict Posttraumatic Stress Disorder Symptom Maintenance After Acute Civilian Trauma. Biological Psychiatry, 81(12), 1023–1029. doi: 10.1016/j.biopsych.2016.11.015
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Surgery Replication. Archives of General Psychiatry, 62, 593–602.
Lanius, R. A., Bluhm, R. L., Hegadoren, K. M., Rowe, B., Theberge, J., et al. (2010). Default mode network connectivity as a predictor of post-traumatic stress disorder symptom severity in acutely traumatized subjects. Acta Psychiatrica Scandinavica, 121, 33–40.
Wingen, G. A. V., Geuze, E., Vermetten, E., & Fernández, G. (2011). Perceived threat predicts the neural sequelae of combat stress. Molecular Psychiatry, 16(6), 664–671. doi: 10.1038/mp.2010.132
Admon, R., Lubin, G., Stern, O., Rosenberg, K., Sela, L., Ben-Ami, H., & Hendler, T. (2009). human vulnerability to stress depends on amygdalas predisposition and hippocampal plasticity. Proceedings of the National Academy of Sciences, 106(33), 14120–14125. doi: 10.1073/pnas.0903183106
Davis, M., & Whalen, P. J. (2000). The amygdala: vigilance and emotion. Molecular Psychiatry, 6(1), 13–34. doi: 10.1038/sj.mp.4000812
Roozendaal, B., McEwen, B. S., & Chattarji, S. (2009). Stress, memory, and the amygdala. Nature Reviews Neuroscience, 10, 423–433.
Heilbronner, S. R., & Hayden, B. Y. (2016). Dorsal Anterior Cingulate Cortex: A Bottom-Up View. Annual Review of Neuroscience, 39(1), 149–170. doi: 10.1146/annurev-neuro-070815-013952
American Psychiatry Association (2000). DSM-IV-TR: Diagnostic and Statistical Manual of Mental Disorders (4th ed.). Washington DC.
Eoa, E. B., & Tolin, D. F. (2000). Comparison of the PTSD Symptoms Scale: Interview Version and the Clinician-Administered PTSD Scale, 181–191.
Beck, A. T., Steer, R. A., & Cabrin, M. G. (1988). Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review, 77– 100.
[+] Other Work By Tori Davis
Schizophrenia and the Leaky Blood Brain Barrier
Neurophysiology
Researchers looked at the relationship between the 22q11.2 deletion syndrome (22qDS) and schizophrenia. Their results showed that 22qDS schizophrenia may be the result of a compromised blood brain barrier (BBB).