Broccoli can prevent psychosis
A new study shows intake of a glucoraphanin dietary prevents sfi1 expression in the medial prefrontal cortex for adult offspring of maternal immune activation.
Author: Vanity Garcia
Download: [ PDF ]
Neuroanatomy
Abstract
Schizophrenia can be determined from genetic vulnerabilities and environmental insults in order to be diagnosed as a neurodevelopmental disorder.1 A genetic abnormality of maternal immune activation can lead into the severe symptoms of schizophrenia disorder.2 Maternal immune activation (MIA) occurs in pregnant women who are at a higher risk of their neonate’s functional connectivity being stressed, inflamed, and weakened.3 MIA increases in glutamatergic synapse and expression of suppressor of fermentation-induced loss of stress resistance protein 1 (SfI1) mRNA from the medial prefrontal cortex.4 In a paper recently published in Scientific Reports, Matsuura and Hashimoto investigated the intake of glucoraphanin prevents sfi1 expression in the medial prefrontal cortex for adult offspring with maternal immune activation.5
Background
Glucoraphanin is the precursor of a sulforaphane antioxidant and found in cruciferous vegetables such as broccoli and cauliflower.5,6 Adults that were offspring of maternal immune activation have been demonstrated to reduce psychosis symptoms with glucoraphanin dietary.5 Psychosis symptoms are a higher risk to develop for adult offspring such as delusional, hallucinations, and cognitive functions.7 Cognitive dysfunctions and environmental stressors have shown to impair prefrontal functions such as maternal immune activation.8
Methods
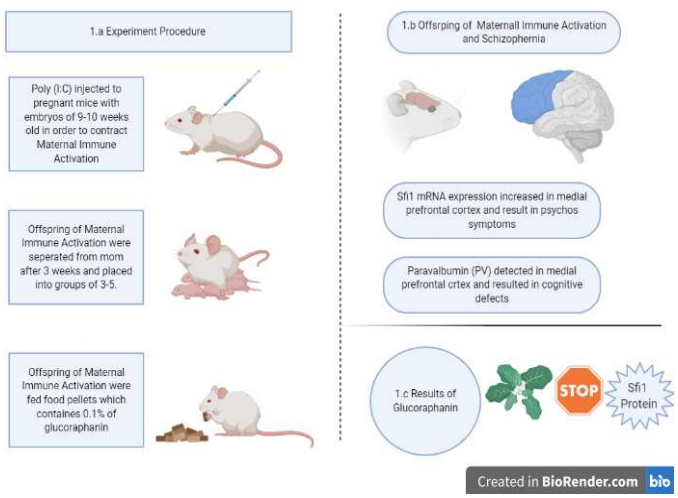
Pregnant mice with embryos of 9-10 weeks old were placed under a controlled polycarbonate cage with a 12/12-hour light-dark cycle. The mice were injected intraperitoneally for 6 consecutive days with poly(I:C) in order to contract MIA in figure 1.a.5 The offspring from their mothers after 3 weeks and caged into 3-5 per group.5 Food pellets contained 0.1% of glucoraphanin were prepared with broccoli sprout extract powder and fed to the offspring in figure 1.a.5 The Sfi1 mRNA expression levels of the offspring’s prefrontal cortex were measured by an RNA extraction using an RNeasy Mini kit.5 Western blot analysis of Sfi1 protein in the medial prefrontal cortex from offspring after maternal immune activation was performed and compared to postmortem brain samples from schizophrenia.5,9 Immunohistochemistry analysis of parvalbumin (PV) in the medial prefrontal cortex from offspring after MIA were observed for cognitive defects in figure 1.b.5
Results
Expression of prenatal poly(I:C) showed a reduction of parvalbumin immunohistochemistry in offspring’s medial prefrontal cortex with MIA compared to the control group. The reduction of PV resulted to cognitive impairment and psychosis.5 The effects of dietary intake of 0.1% glucoraphanin food pellets on adult offspring after MIA resulted in improved cognitive deficits. Another PV immunohistochemistry was performed on adult offspring of MIA with a dietary intake of glucoraphanin had a significantly higher amount of PV within the medial prefrontal cortex than the control group.5 The RNA sequencing of the prefrontal cortex in adult offspring resulted in a significant change of suppressor of fermentation-induced loss of stress resistance (sfi1) expression.5 The sfi1 mRNA expression in the prefrontal cortex was increased by the poly(I:C) injection and the dietary intake of glucoraphanin blocked the increase of the sfi1 gene expression shown in figure 1.c.5 The Sfi1 protein in schizophrenia was significantly higher than the control group.5 Sfi1 mRNA expression in hair follicles of schizophrenia were significantly lower than the healthy control group.5
Conclusion
Maternal immune activation is an infection-induced during pregnancy from a cascade of cytokines and immunologic alterations are transmitted to the fetus. MIA strikes the central nervous system and causes a neurochemical and anatomic changes in the brain.11 These changes result into psychosis symptoms and schizophrenia disorder in the adult offspring after MIA.10 This study explored how to reduce the psychosis symptoms in the adult offspring after maternal immune activation by using a dietary intake of glucoraphanin. Intaking 0.1% of glucoraphanin for offspring after MIA prevented cognitive deficits and reduction of parvalbumin in the medial prefrontal cortex. The Sfi1 expression aided in the development of behavioral abnormalities in adult offspring, which were blocked by the glucoraphanin intake.5 Comparing the sfi1 mRNA in hair follicles of schizophrenia mice to sfi1 protein in the postmortem brain expressed how sfi1 associates to the pathophysiology of schizophrenia.5 This study reveals how adolescences are more vulnerable to psychiatric disorders and how psychosis symptoms can be prevented during this time period.5 Looking into more nutritional antioxidants that can prevent psychosis for schizophrenia disorder can benefit future research.
[+] References
Alvarez, R. J., Pafundo, D. E., Zold, C. L., & Belforte, J. E. (2020, April 15). Interneuron NMDA Receptor Ablation Induces Hippocampus-Prefrontal Cortex Functional Hypoconnectivity after Adolescence in a Mouse Model of Schizophrenia. Retrieved April 16, 2020, from https://www.jneurosci.org/content/40/16/3304
Dickerson, D. D., Wolff, A. R., & Bilkey, D. K. (2010, September 15). Abnormal Long-Range Neural Synchrony in a Maternal Immune Activation Animal Model of Schizophrenia. Retrieved April 16, 2020, from https://www.jneurosci.org/content/30/37/12424
Spann, M. N., Monk, C., Scheinost, D., & Peterson, B. S. (2018, March 14). Maternal Immune Activation During the Third Trimester Is Associated with Neonatal Functional Connectivity of the Salience Network and Fetal to Toddler Behavior. Retrieved April 16, 2020, from https://www.jneurosci.org/content/38/11/2877
Li, Y., Missig, G., Finger, B. C., Landino, S. M., Alexander, A. J., Mokler, E. L., … Bolshakov, V. Y. (2018, March 2 8). Maternal and Early Postnatal Immune Activation Produce Dissociable Effects on Neurotransmission in mPFC–Amygdala Circuits. Retrieved April 16, 2020, from https://www.jneurosci.org/content/38/13/3358
Matsuura, A., Ishima, T., Fujita, Y., Iwayama, Y., Hasegawa, S., Kawahara-Miki, R., … Hashimoto, K. (2018, February 1). Dietary glucoraphanin prevents the onset of psychosis in the adult offspring after maternal immune activation. Retrieved April 16, 2020, from https://www.nature.com/articles/s41598-018-20538-3#Abs1
Zhao, J., Moore, A. N., Redell, J. B., & Dash, P. K. (2007, September 19). Enhancing Expression of Nrf2-Driven Genes Protects the Blood–Brain Barrier after Brain Injury. Retrieved April 16, 2020, from https://www.jneurosci.org/content/27/38/10240
Malkova, N. V., Yu, C. Z., Hsiao, E. Y., Moore, M. J., & Patterson, P. H. (2012, January 29). Maternal immune activation yields offspring displaying mouse versions of the three core symptoms of autism. Retrieved April 19, 2020, from https://www.sciencedirect.com/science/article/abs/pii/S088915911200013X?via=ihub
Xu, X., Chini, M., Bitzenhofer, S. H., & Hanganu-Opatz, I. L. (2019, February 13). Transient Knock-Down of Prefrontal DISC1 in Immune-Challenged Mice Causes Abnormal Long-Range Coupling and Cognitive Dysfunction throughout Development. Retrieved April 16, 2020, from https://www.jneurosci.org/content/39/7/1222
Han, M., Zhang, J.-C., & Hashimoto, K. (2017, February 28). Increased Levels of C1q in the Prefrontal Cortex of Adult Offspring after Maternal Immune Activation: Prevention by 7,8-Dihydroxyflavone. Retrieved April 19, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5290721/
Knuesel, I., Chicha, L., Britschgi, M., Schobel, S. A., Bodmer, M., Hellings, J. A., … Prinssen, E. P. (2014, October 14). Maternal immune activation and abnormal brain development across CNS disorders. Retrieved April 19, 2020, from https://www.nature.com/articles/nrneurol.2014.187
Minakova, E., & Warner, B. B. (2018, November 14). Maternal immune activation, central nervous system development and behavioral phenotypes. Retrieved April 16, 2020, from https://onlinelibrary.wiley.com/doi/full/10.1002/bdr2.1416
[+] Other Work By Vanity Garcia
Dyno Tuning Your Neurons
Neurophysiology
A new study shows implanting artificial neurons into the brain can be used as a deep brain stimulator treatment to restore failing brain circuits within neurodegenerative disease. The artificial neurons and synapses can be linked to machines and be controlled over the internet.